

Postpartum blood sugar after gestational diabetes: What to expect, what’s normal, and when to take a deep breath.
You made it through pregnancy with gestational diabetes. The finger pricks, the food tracking, the carb math — all behind you, right?
Well… mostly. For many, blood sugar levels return to normal within days of delivery. But that doesn’t mean you're done caring for your health — or that gestational diabetes didn’t leave lasting questions or emotional imprints.
This post walks you through:
What typically happens to blood sugar after birth
How to know if yours is back to normal
When (and why) to follow up
How to support your postpartum blood sugar and well-being
Once the placenta is delivered, the hormones that caused insulin resistance—like human placental lactogen and cortisol—drop rapidly. This often leads to a sudden improvement in insulin sensitivity.
Research shows that ~95% of people with gestational diabetes return to normal blood glucose levels within a few days postpartum.
But that doesn’t mean everything snaps back perfectly. In the early stages after delivery, blood sugar regulation can be unpredictable. In those early days:
You might be eating at odd times
You’re sleep-deprived
You’re under stress (hello, newborn life)
You might not know what to eat anymore
All of that can affect your numbers, mood, and recovery.
The early postpartum period is significant for monitoring baby's blood glucose levels, as this is a critical window for detecting and managing any issues. Checking the baby's blood glucose level is standard practice after birth, especially if the mother had gestational diabetes.
Even if your blood sugar normalizes, it’s important to follow up with your healthcare provider. Postpartum glucose testing is recommended for all women who experienced gestational diabetes mellitus, as they are at higher risk of developing type 2.
Here’s what most guidelines (like ACOG and ADA) recommend:
6–12 weeks postpartum: Take a 2-hour oral glucose tolerance test (OGTT), which includes both fasting plasma glucose (before drinking the solution) and a measurement at two hours (after drinking the solution). Impaired fasting glucose or impaired glucose tolerance may be diagnosed based on these results.
Results are interpreted as:
Impaired fasting glucose (IFG): fasting 100–125 mg/dL
Impaired glucose tolerance (IGT): 2-hour 140–199 mg/dL
Diabetes: fasting ≥126 mg/dL or 2-hour ≥200 mg/dL
Every 1–3 years after: Routine screening, especially if you have risk factors or have previously been tested for glucose intolerance.
Why?
Because up to 50% of people who had gestational diabetes will develop type 2 diabetes within 10 years.
It’s not about panic — it’s about prevention and early support. Knowing your risk is power.
After delivery, here’s what your numbers should look like (based on ADA criteria):
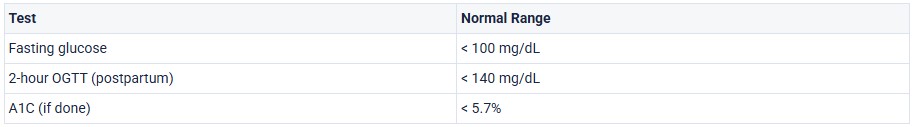
If your numbers are above these ranges, you may be diagnosed with prediabetes or type 2 diabetes.
But if they’re in the gray zone, don’t panic — your provider may retest or suggest lifestyle adjustments first.
Even if gestational diabetes is “over,” your body’s still adjusting. These factors can affect glucose:
Breastfeeding – often lowers blood sugar, but if you don’t eat enough, it can cause dips
Lack of sleep – increases cortisol, which raises blood sugar
Stress – emotional and physical stress affect glucose regulation
Nutrition swings – skipping meals or relying on quick carbs can spike levels; focusing on a balanced diet is important for stabilizing blood sugar after delivery
Hormonal changes – estrogen and progesterone shifts impact insulin sensitivity
Obesity, including pre-pregnancy BMI and postpartum weight gain, can also make postpartum blood sugar regulation more challenging.
In other words: you’re human. Fluctuations don’t mean failure — they mean your body is healing and recalibrating.
Eat balanced meals regularly
Pair carbs with protein or fat
Move your body gently — even short walks help
Stay hydrated — especially when breastfeeding
Prioritize sleep where you can
Check in on your mental health
Schedule that follow-up test — and repeat as recommended
Gestational diabetes often feels like a pregnancy-only problem. But for many of us, it lingers — not just in numbers, but in memories, habits, and health decisions.
Even after baby is born, you’re still worth checking in on. Your long-term health matters. And you deserve care that continues, not just care that stops at delivery.
1. How long does blood sugar stay high after birth?
For most people, blood sugar levels drop quickly after delivery, often within 24–72 hours. That’s because the placenta — the source of insulin resistance — is no longer in the body. But if your numbers were very high during pregnancy or you used insulin, it might take a little longer.
If your blood sugar remains elevated, it’s important to follow up. This could signal ongoing insulin resistance or prediabetes.
2. What are normal postpartum glucose levels after gestational diabetes?
“Normal” means your body can handle sugar without spiking above safe levels. For most, fasting glucose should be under 100 mg/dL, and 2-hour post-meal glucose under 140 mg/dL, though labs may vary slightly.
Your doctor will confirm this with the gestational diabetes follow-up test, usually done between 6–12 weeks postpartum.
3. Do I need to keep checking my blood sugar after giving birth?
Not necessarily. Most people can stop daily finger-stick testing unless otherwise advised. However, if you feel symptoms like fatigue, shakiness, or headaches — or you're just curious — it’s okay to check occasionally during recovery.
Some find comfort in briefly tracking postpartum glucose levels after gestational diabetes — especially while adjusting to a new routine or breastfeeding.
4. What is the gestational diabetes follow-up test (postpartum glucose test) — and do I need it?
Yes. The 2-hour OGTT (oral glucose tolerance test) is recommended around 6–12 weeks postpartum. This test evaluates your current glucose metabolism and helps your doctor see if you’ve returned to normal, developed prediabetes, or are at risk of type 2 diabetes.
Even if you feel fine, this test matters — because not all changes are visible or felt right away.
5. What’s my risk of type 2 diabetes after GDM?
Having had GDM does increase your chances of developing type 2 diabetes later in life. Research shows that up to 1 in 3 people with gestational diabetes may have some level of insulin resistance after birth.
That’s why it’s essential to stay on top of your health — with regular glucose testing every 1–3 years, balanced meals, movement, and stress support.
6. If my numbers are normal now, do I still need to worry about type 2 diabetes later?
You don’t need to “worry,” but you should stay proactive. Gestational diabetes is a major risk factor, so continue regular screening every 1–3 years.
7. Can I get gestational diabetes again in a future pregnancy?
Yes — your risk increases if you've had it before. That’s why early screening is often recommended in future pregnancies.
8. Is breastfeeding helpful for blood sugar?
Yes! Breastfeeding is associated with lower postpartum glucose levels and a reduced risk of developing type 2 diabetes. But you’ll need more calories and consistent meals.
9. What if my postpartum test shows prediabetes or type 2 diabetes?
You’re not alone. Many people catch this early thanks to the follow-up test. Most providers will start with lifestyle support, and in some cases, medication if needed.
10. How can I support my blood sugar postpartum — especially while breastfeeding?
Postpartum recovery takes energy — especially if you’re nursing. To stay stable:
Include protein and fat with your carbs
Eat every 2–4 hours (especially during cluster feeds)
Stay hydrated
Try gentle movement like short walks
11. What should I ask my doctor at my 6-week check-up?
Here are a few good questions:
“Can we go over my postpartum glucose test results?”
“Do I need ongoing testing or follow-up?”
“Should I be concerned about Type 2 diabetes?”
“Is it okay to ease off meal tracking now?”
Bring any lingering questions — you deserve full care, not just a quick discharge.
Get a Free 20-Day Shopping List